What is coeliac disease?
Coeliac disease is one of the most under diagnosed medical conditions in Australia. It is estimated up to 200,000 Australians have coeliac disease and don't even know it, with many of these being children.
Coeliac disease is the result of an autoimmune response triggered by a protein found in gluten-containing foods. The presence of gluten causes the walls of the intestines to become inflamed and damages the delicate 'finger-like' cells (microvilli) that line our gut wall. As a result, microvilli become flattened and reduce our ability to absorb vitamins and minerals from our food.
Healthy microvilli Flattened and damaged microvilli
Constant exposure to gluten causes prolonged intestinal inflammation and may lead to the following symptoms:
• Abdominal pain
• Bloating
• Constipation and/or diarrhoea
• Sore joints
• Eczema or other skin irritations
• Weak muscles
• Poor hair growth
• Poor appetite/fussy eaters as children
• Mouth ulcers
• Halitosis or bad breath
• Undigested food in stools
• Fatigue
• Vitamin deficiencies, such as; iron and B12
If left untreated, coeliac disease has many long-term effects on our health, including; an increased risk of bowel cancer, osteoporosis, chronic vitamin deficiency and muscle wastage (atrophy) from a lack of protein absorption.
Coeliac disease is initially diagnosed by a blood test aimed at detecting Anti-Gliadin antibodies (gliadin is the gluten protein found in wheat) and HLA-B8 and HLA-DQ2 genes. If these tests return a positive reading for antibodies or genes are detected, a small bowel biopsy will be performed to confirm the presence of the disease. If the biopsy returns positive, the patient will need to follow a gluten free diet for life.
It is recommended that if you suspect you have coeliac disease, do not stop eating gluten, as the suspected allergen needs to be present in the body in order for the tests to give a 'true positive' result. It is important to discuss symptoms with a health practitioner before making any changes to your diet.
Why did I go Gluten Free?
I decided to take on the 30-day gluten free challenge to better understand the challenges facing a newly diagnosed coeliac patient. I avoided all foods containing gluten, including packaged items stating 'may contain traces of gluten'.
Week 1
As a qualified Nutritionist, I inform my patients that a diet change is not just a matter of altering your food choices, it involves a change in mindset. Being organised and motivated from the beginning is a crucial step in succeeding.
I began by creating a list of all the foods I consume that contain gluten. I recommend that all newly diagnosed coeliac individuals do the same. This process helps to put things into perspective. Aside from the obvious bread, pasta and grains, I continued with sauces, spreads, protein powders and spice mixes. The end resulted in a long list.
After stocking up on groceries, I began meal prepping for the week. Preparation is an important step that will save you falling back into old habits or getting stuck when there are no gluten free options in sight.
I prepared chia puddings and overnight quinoa porridge for breakfast, packed tubs of raw nuts for snacks and my lunch and dinners consisted of a protein base with a large salad of vegetables and herbed quinoa.
Week 2
I struggled with meal prepping for the week. At the start of the week, I forgot to make lunch and by 12pm I was famished. I made a quick dash to the local market, where I bought a gluten free chicken salad, all the while staring longingly at the fresh crusty bread rolls and sweet smelling croissants on offer at the counter, it was then when I learnt my lesson. I made a mental note to put aside time and meal prep my lunches for the rest of the week. I'm sure most people working full time will understand that lunch is commonly the biggest hurdle we face during the working week. My advice is, prepare, prepare, prepare.
It was in week two that I purchased packaged gluten free options, such as; bread and pasta.
Having had quinoa for seven days straight, I was fairly sick of it. I craved pasta (one of my original staples), I decided to try a rice and corn spaghetti in a basic tomato sauce. The pasta cooks faster than normal semolina, so I advise you to keep a close eye on it. This pasta had a pleasant taste, the texture holds up very well and it did not leave me with a bloated stomach.
It was in week two that I attended a birthday party. When the cake arrived, I was so close to giving in and taking a slice. I quietly asked, 'is it gluten free?' however, by the response of the host I decided to have a cup of tea instead, trying to block out the joyful screams of content coming from the cake eaters. This does not mean you need to eat cake to enjoy or celebrate a party, however, to have the 'option' to join in is something I believe most coeliac sufferers are familiar with.
Week 3
Breakfasts consisted of smoothies, loaded with fruit, almond milk, coconut yoghurt and gluten free protein powder. I am consuming more wholefoods in my diet, such as; raw nuts and seeds, pineapples and red and dark green leafy vegetables. I have introduced a probiotic to help maintain gut health and I feel along with the removal of gluten, my gut is in a much better state.
Lunch consists of quinoa salads with raw almonds, currants, rocket leaves and citrus dressing. I am rotating the vegetables I use to keep the meals interesting.
This week the real challenge was eating out. When booking a dinner, I advised the restaurant that I required gluten free options. When I arrived, I sadly found that only one main meal was completely gluten free and no dessert. I sat envious of my companions chocolate brownie, with just a cup of tea to end the meal. I definitely recommend reviewing a menu in advance if possible. If I had seen the menu before I booked a table, I would have suggested a different restaurant.
Surprisingly, the next day was far more enjoyable. At a nearby café, I asked whether they had gluten free options available. I was told by the waiter that they had fresh gluten free bread. It was exciting to be told there are gluten free options on the menu.
I had a newfound understanding for coeliac sufferers, it may seem straightforward, however, the amount of options available when eating out is minuscule. I can see the shift to accommodate food intolerances, however, more awareness is needed.
As for my personal update, my gastrointestinal discomfort has reduced, almost no bloating after a meal and more energy. This is very pleasing to me. I feel as though all my efforts are really paying off. I am also considering reducing the amount of gluten foods in my diet, even after this month is over.
Week 4
I am excited, not relieved to be approaching the end of my 30-day challenge.
I developed a new routine; meal prepping for the week, finding gluten free recipes to make for special occasions and preparing healthier meals. I have introduced my friends and family members to some new products and now gluten free pasta and quinoa is a new pantry staple in our home.
This week I was pleasantly surprised when I was presented with gluten free crackers bought specially for me by a work colleague for a morning snack – it was very thoughtful and normally not something a person would appreciate so much. Having a food intolerance does give you a new appreciation for food and for someone else to consider that on your behalf, can make socialising a lot more enjoyable.
My final grocery shop, I found myself thinking of how much better I felt after eliminating gluten. Once I established a routine, I found that 'living gluten free' could be a sustainable change and one that I will be maintaining after this challenge.
For newly diagnosed coeliacs, I advise you to do your research and be aware that this is a lifestyle change as well as a dietary one. Be sure to consider that gluten can be found in many products besides food, including; medications, supplements and even beauty products.
I end my month by summarising the common challenges I came across and provided a table of foods to include and avoid for newly diagnosed coeliac individuals.
Challenges
Eating out: When I booked a table at a restaurant or café, I was required to ask whether gluten free options were available. Whilst difficult initially, I did adjust quite well. I now understand this to be a common challenge, however, as awareness grows, I anticipate more establishments will include and increase gluten free options.
Cost: The cost of groceries seemed slightly more and I even came across a restaurant that charged more for gluten free bread. I recommend taking the time to research – compare price points and consider joining a loyalty program, as many stores offer their customers member discounts.
Label checking: I was constantly checking labels on all products that I purchased. I was surprised to see that gluten is present in many everyday items, such as; sauces, dressings, spreads, packaged salads, pre-marinated meats and burger patties. I recommend talking to your butcher or shop at your local fruit market to get a fresh supply of fruit and vegetables.
Special occasions: Social gatherings posed a challenge. I couldn't eat a slice of birthday cake or salad that had store bought dressing on it. In these situations, I found it easier to offer to make something for the special occasion, that way I was able to join in.
Cooking and lifestyle tips
• Pantry overhaul: Examine all packaged foods for gluten to minimise the chance of 'accidently' ingesting it.
• Familiarise yourself with your local health food store and health food section of your supermarket. Weekend markets have great stalls selling boutique products that are gluten free - ask for staff members' help and advice, they are a wealth of knowledge and you might pick up some cooking tips too.
• Make a shopping list before heading out – don't deviate and you will reduce your costs and time spent shopping.
• Replace wheat flour in your pantry with gluten free flour. Plain and self-raising are readily available and work very well for crumbing, baking, binding and use in batters.
• Make food interesting by using gut loving herbs and spices to add flavour to dishes such as cinnamon, ginger, turmeric and bitter greens.
• Eat a rainbow – remember to not compromise your food choices just because you are cutting out staples – find alternatives and maintain the quality of your food.
• Don't skip meals – a handful of nuts or a piece of fruit is better than going hungry.
• Advise restaurants at the time of booking that you require gluten free options as most places are mindful and happy to accommodate food intolerances.
• A common belief is that gluten free means 'healthy' – beware, this is not always the case. Many gluten free products have added sugars, so please check your labels, and remember sugar is as inflammatory to a coeliac as gluten is.
• Make an appointment to see a nutritionist – they can advise you on dietary requirements, provide recipes, and develop treatment plans to help minimise the symptoms of intestinal inflammation.
Foods to avoid and foods to include:
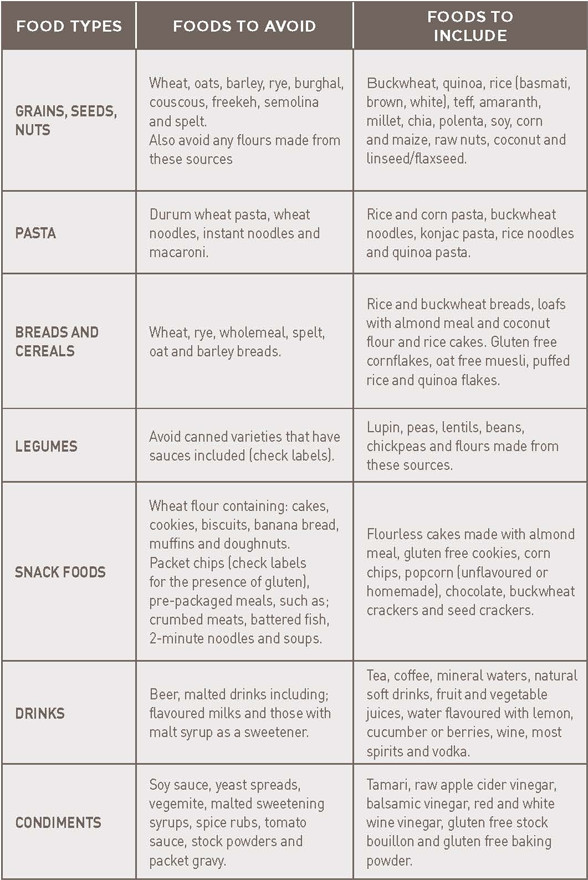
Due to the nature of gluten being present in small amounts in packaged foods, it is recommended that you check labels and familiarise yourself with gluten sources.
In the past month, I have learnt that I do not need to eat gluten foods, nor did I necessarily miss them. Yes, I craved a piece of birthday cake (and almost gave in!) and yes, a slice of hot toast with vegemite would be wonderful at 6am for breakfast. However, my cravings went away just as fast as it came and I was left feeling happy, without the bloated stomach.
I was happy to find restaurants and cafes were making the effort to cater for the diverse dietary requirements of patrons, something I believe larger chains might want to take on board. Overall, it seems the major concern for coeliac sufferers seems to be the cost factor – gluten free products can be higher in price than their gluten containing equivalent. For the newly diagnosed coeliacs, I recommend you get in contact with a support group like the Coeliac Society. They are a fantastic source of knowledge and can make the gluten free transition a seamless one.
If you feel that you may be suffering from gluten intolerance or coeliac disease, it is recommended you visit your healthcare practitioner. Remember, it is not recommended you embark on a gluten free diet without seeking medical advice, nor begin a diet without the proper medical testing.
For more information about coeliac disease, the Coeliac Society has branches for every Australian state and provide up to date information for coeliacs.
Please visit: www.coeliac.org.au
For help locating an accredited nutritionist, please visit: www.australiannaturaltherapistsassociation.com.au or www.naturaltherapypages.com.au
What is Gluten?
Gluten is a storage protein found in grains. Gluten is found in different forms, most commonly:
• Secalin in rye • Gliadin in wheat • Avenin in oats • Hordein in barley
For many of us, consuming these foods does not cause any symptoms. However, for an ever growing number of the population, intolerance to gluten is the cause of many health problems and they aren't aware of it.
By Ayse Halil
Kadac Customer Service Representative & Nutritionist

